Dry cupping and wet cupping are related but distinct therapies that use suction to stimulate circulation and relieve pain, with dry cupping remaining non-invasive and wet cupping involving controlled skin incisions and blood removal, resulting in different risk profiles and treatment considerations.
Cupping therapy has moved from traditional healing systems into mainstream wellness, sports medicine, and integrative care settings. Despite its growing visibility, many patients remain unclear about the difference between wet cupping and dry cupping and which option is appropriate for their condition.
Both techniques rely on negative pressure applied to the skin, yet they diverge sharply in invasiveness, physiological impact, and safety requirements. Understanding how each method works, what benefits are realistically supported, and where risks increase is essential before choosing a treatment approach.
Key Takeaways
- Dry cupping is non-invasive and generally safer for routine muscle pain and tension
- Wet cupping involves bloodletting and carries higher infection and recovery risks
- Evidence supports short-term pain relief for both methods, with limited proof of detoxification claims
- Wet cupping should be used selectively and only by trained professionals
- Cupping is a complementary therapy and not a substitute for medical care
What Is Cupping Therapy
Cupping therapy is a complementary treatment that uses suction on the skin to stimulate blood flow, relax muscle tissue, and influence pain signaling.
Cupping has been practiced across multiple cultures for centuries, including East Asian medicine, Middle Eastern hijama traditions, and early European bloodletting practices. Modern applications are more controlled and often integrated into physical therapy, acupuncture, and sports recovery programs.
Physiologically, cupping creates localized negative pressure that lifts skin and superficial tissue layers. This decompression contrasts with compression-based therapies like massage and may influence circulation, fascia mobility, and nervous system responses.
Dry Cupping Explained
Dry cupping uses suction on intact skin to reduce muscle tension, improve mobility, and provide short-term pain relief without breaking the skin.
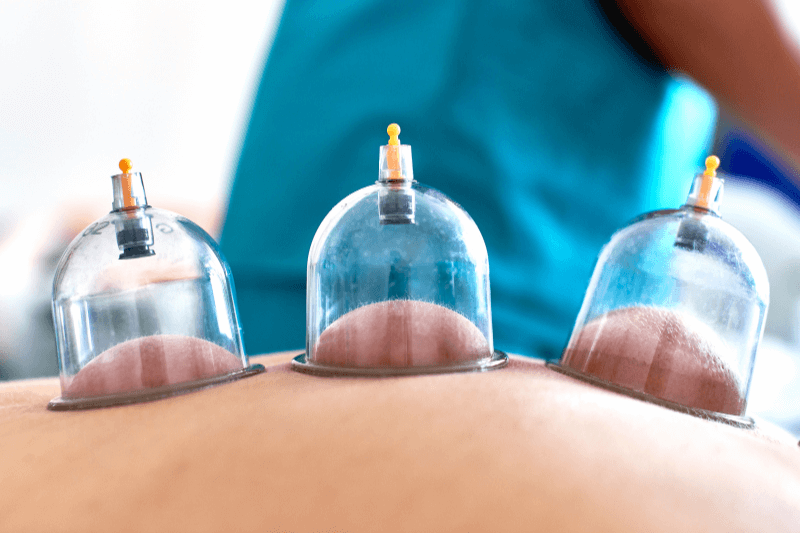
Dry cupping involves placing cups on the skin and creating a vacuum using manual pumps, heat, or flexible silicone cups. The skin and underlying tissue are drawn upward, creating a pulling sensation that many patients describe as intense but tolerable.
Benefits Supported by Evidence
Research suggests dry cupping may offer short-term relief for musculoskeletal pain, particularly in the neck, shoulders, and lower back. Improvements in range of motion and reduced muscle guarding have also been observed, especially in athletic and rehabilitation settings.
Typical Use Cases
- Muscle tightness
- Sports recovery
- Postural strain
- Stress-related tension
- First-time cupping patients
Wet Cupping Explained
Wet cupping adds controlled superficial skin incisions to suction, allowing small amounts of blood to be drawn out, which increases invasiveness and risk.
Wet cupping begins similarly to dry cupping, but after initial suction, the practitioner makes very small, shallow incisions before reapplying suction. This draws out a limited amount of blood and tissue fluid.
Traditional systems describe this process as removing stagnant or unhealthy blood. From a modern medical perspective, wet cupping likely triggers localized inflammatory and immune responses rather than true detoxification.
Claimed Benefits and Limitations
Some small studies suggest potential benefits for chronic pain, migraines, and inflammatory conditions, but the overall quality of evidence remains low. Results vary widely based on technique, frequency, and practitioner skill.
Wet Cupping vs Dry Cupping: Key Differences Explained
Although both methods use suction to influence circulation and tissue response, dry cupping and wet cupping differ significantly in invasiveness, physiological impact, and safety requirements. Understanding these differences helps set realistic expectations and supports informed treatment decisions.
Dry cupping
- Performed on intact skin without incisions
- Uses suction to lift skin and superficial tissues, promoting muscle relaxation and temporary pain relief
- Does not involve blood removal or open wounds
- Carries a low risk of infection when performed correctly
- Typically causes temporary skin discoloration that fades within days
- Requires little to no recovery time
- Commonly used for muscle tension, stiffness, sports recovery, and stress-related discomfort
- Generally appropriate for first-time cupping patients and those seeking a lower-risk option
Wet cupping
- Includes controlled, superficial skin incisions followed by suction
- Draws a small amount of blood and tissue fluid from the surface
- More invasive and requires strict hygiene and sterile technique
- Carries higher risks, including infection, delayed healing, and dizziness
- Requires post-treatment wound care and longer recovery time
- Traditionally associated with chronic or inflammatory conditions, though evidence remains limited
- Not suitable for everyone and usually avoided in beginners, individuals with bleeding risks, or poor wound healing
How to choose the appropriate approach
For most people, dry cupping provides meaningful symptom relief with fewer risks and minimal downtime. Wet cupping should only be considered when its added invasiveness is clearly justified and performed by a properly trained professional following medical screening.
When applied appropriately, cupping therapy can support pain management and mobility, but it should always complement, not replace, comprehensive medical or rehabilitative care.
Benefits Shared by Both Methods
Both cupping methods may reduce pain, improve local circulation, and promote relaxation through nervous system modulation.
Suction dilates local blood vessels and stimulates sensory nerves, which may contribute to pain reduction and relaxation. Many patients report a calming effect similar to deep tissue bodywork.
Risks and Side Effects
Cupping is generally low risk when performed correctly, but wet cupping introduces additional risks related to skin injury and blood exposure.
Common Effects
- Circular skin discoloration
- Mild soreness
Dry Cupping Specific Risks
- Burns when fire is used
- Blistering from excessive suction
Wet Cupping Specific Risks
- Infection
- Scarring
- Dizziness or fainting
- Rare anemia with excessive frequency
Who Should Avoid or Use Caution
People with bleeding disorders, compromised immunity, poor wound healing, or pregnancy-related risks should avoid or carefully evaluate cupping therapy.
Wet cupping is particularly unsuitable for individuals taking blood thinners, those with diabetes-related healing issues, or anyone prone to fainting.
Treatment Planning and Professional Standards
Safe cupping requires trained practitioners, informed consent, and strict hygiene, especially for wet cupping.
Sessions typically last 5 to 20 minutes. Wet cupping demands sterile, single-use instruments and proper post-treatment wound care instructions.
Aftercare and Recovery
After cupping therapy, proper aftercare helps reduce irritation, supports tissue recovery, and lowers the risk of complications.
General aftercare for all cupping treatments
- Protect treated areas from excessive friction or pressure
- Avoid heat exposure, including hot showers, saunas, and heating pads, for at least 24 hours
- Refrain from intense exercise or heavy lifting on treated areas for 24 hours
- Keep the skin clean and dry
- Monitor for unusual pain, swelling, redness, or signs of infection
Cupping marks
- Circular marks or discoloration are common and expected
- Marks are caused by localized capillary response, not bruising from trauma
- Color and intensity vary based on suction strength and individual circulation
- Most cupping marks fade within a few days to two weeks
- Marks should gradually lighten and should not blister or break the skin
Additional care for wet cupping
- Keep incision sites clean, dry, and covered as instructed
- Avoid soaking the area until the skin has healed
- Follow all wound-care guidance provided by the practitioner
- Seek medical advice if signs of infection develop, such as increasing redness, warmth, discharge, or fever
Choosing the Right Option
Dry cupping is appropriate for most muscle-related complaints, while wet cupping should be reserved for specific chronic conditions under professional guidance.
For most patients, dry cupping offers meaningful benefits without unnecessary risk. Wet cupping should only be considered when its added invasiveness is justified and medically appropriate.
FAQs
1. How often should wet cupping or dry cupping be done?
Dry cupping can typically be performed more frequently, often once per week or every two weeks, depending on muscle recovery and symptom severity. Wet cupping requires longer intervals between sessions due to skin healing and blood loss and is usually limited to occasional treatments spaced several weeks apart. Frequency should always be determined by practitioner assessment and patient response.
2. Does wet cupping remove toxins from the body?
There is no strong scientific evidence showing that wet cupping removes toxins from the bloodstream. The blood drawn during wet cupping is peripheral capillary blood, not stored or toxic blood. Any perceived benefit is more likely related to localized inflammatory, immune, or nervous system responses rather than true detoxification.
3. Is cupping therapy painful?
Cupping is generally described as uncomfortable rather than painful. Dry cupping creates a strong pulling or pressure sensation that subsides quickly. Wet cupping may involve brief discomfort during skin incisions, but pain is usually minimal when performed correctly. Pain tolerance varies by individual and treatment area.
4. Can cupping therapy be combined with acupuncture or physical therapy?
Yes. Cupping is commonly used alongside acupuncture, physical therapy, massage, and rehabilitation programs. Dry cupping is especially compatible with movement-based therapies, as it may improve tissue mobility before or after exercise. Coordination between providers ensures safe and effective integration.
5. How long do cupping marks last?
Cupping marks typically last between a few days and two weeks. Duration depends on suction strength, treatment duration, and individual circulation. Marks from wet cupping may last slightly longer due to skin incisions and localized inflammation, but they should gradually fade without scarring when properly cared for.
Care Integration and Next Steps
Wet cupping and dry cupping share a common foundation but serve different purposes and risk profiles. Dry cupping remains the safer, more accessible option for managing muscle tension and pain, while wet cupping requires careful screening, advanced training, and clear clinical justification. When used appropriately, cupping functions best as a supportive therapy within a broader, well-structured care plan rather than as a standalone intervention.
At ACA Acupuncture and Wellness, we offer cupping therapy as part of our individualized, integrative approach to care. Our treatment plans may also include acupuncture services, TuiNa massage, Chinese herbal medicine, physiotherapy treatment, facial acupuncture, moxibustion, reflexology, ear seeding, and thermal therapy. We base every recommendation on the patient’s condition, clinical presentation, and long-term health goals, with a strong emphasis on safety, appropriateness, and coordinated care.
If you are considering cupping therapy or exploring integrative treatment options for pain management, mobility concerns, or overall wellness support, contact us at ACA Acupuncture and Wellness to schedule a consultation and discuss which therapies may be most suitable for your needs.
Sources:
Furhad, S., Sina, R. E., & Bokhari, A. A. (2023). Cupping therapy. In StatPearls. StatPearls Publishing.
Cleveland Clinic. (2023, June 7). Cupping therapy.
Ugur, N. K., Tursunbadalov, S., Sargun, S., Welcome, M. O., & Dane, S. (2018). The effects of wet cupping therapy on the blood levels of some heavy metals: A pilot study. Journal of Acupuncture and Meridian Studies, 11(6), 375–379.
Sohrabi, F., Tirgari, B., Forouzi, M. A., Roy, S. C., Tajadini, H., Jahani, Y., & Seifaddini, R. (2025). Effectiveness of dry cupping therapy on fatigue and quality of life of women with multiple sclerosis: Randomized clinical trial. Iranian Journal of Nursing and Midwifery Research, 30(6), 815–822.






Recent Comments