Restless Leg Syndrome Relief: Natural Ways to Reduce Urges, Tingling, and Nighttime Restlessness
Restless Leg Syndrome, often shortened to RLS, is frequently misunderstood and mistreated because it does not behave like a typical muscle or sleep disorder. Many people are told to stretch more, exercise harder, or simply “deal with it,” yet symptoms persist night after night. The frustration comes from the fact that RLS is driven by the nervous system, not the legs themselves.
Symptoms almost always worsen in the evening or at night because that is when key neurological processes shift. Dopamine levels drop, the brain attempts to downshift into rest mode, and any instability in nerve signaling becomes far more noticeable. Understanding this timing is critical, because effective relief depends on working with the nervous system rather than fighting it.
Restless Leg Syndrome Relief: Natural Ways to Reduce Urges, Tingling, and Nighttime Restlessness
Restless Leg Syndrome, often shortened to RLS, is frequently misunderstood and mistreated because it does not behave like a typical muscle or sleep disorder. Many people are told to stretch more, exercise harder, or simply “deal with it,” yet symptoms persist night after night. The frustration comes from the fact that RLS is driven by the nervous system, not the legs themselves.
Symptoms almost always worsen in the evening or at night because that is when key neurological processes shift. Dopamine levels drop, the brain attempts to downshift into rest mode, and any instability in nerve signaling becomes far more noticeable. Understanding this timing is critical, because effective relief depends on working with the nervous system rather than fighting it.
Key Takeaways
- Restless Leg Syndrome is a neurological condition, not a circulation or muscle problem.
- Nighttime symptoms are linked to dopamine rhythms and low brain iron availability.
- Lifestyle and sleep timing adjustments can significantly reduce symptom severity.
- Nutrients such as iron, magnesium, and vitamin B12 only help when deficiencies are present.
- Acupuncture supports nervous system regulation and improves sleep quality over time.
What Restless Leg Syndrome Actually Is
Restless Leg Syndrome is defined as a sensory-motor neurological disorder characterized by an uncontrollable urge to move the legs, usually accompanied by uncomfortable sensations such as tingling, pulling, buzzing, or crawling. These sensations typically appear or worsen during periods of rest, improve with movement, and are most intense in the evening or at night.
In clinical practice, diagnosis is based on symptom patterns rather than imaging or blood tests alone. The core diagnostic criteria include:
- An urge to move the legs, often with unpleasant sensations
- Symptoms that begin or worsen during rest or inactivity
- Partial or complete relief with movement
- Symptoms that are worse in the evening or at night
RLS is often confused with other conditions, which delays proper treatment. Leg cramps cause sudden, painful muscle tightening rather than an urge to move. Peripheral neuropathy causes numbness or burning that does not reliably improve with movement. Anxiety-related restlessness is typically generalized and not limited to the legs or nighttime hours.
Why Symptoms Appear at Night
RLS symptoms intensify at night because the brain shifts into a different regulatory mode over the 24-hour cycle. In the evening, the nervous system is meant to downshift into rest, but in people with RLS, this transition is unstable.
- Dopamine levels naturally decline at night, reducing the brain’s ability to filter unnecessary movement and sensory signals.
- Unstable dopamine signaling becomes more noticeable during rest, which is why symptoms worsen when lying still.
- Iron is essential for dopamine production and transport in the brain, not just in the bloodstream.
- Brain iron can be low even when blood tests look normal, weakening dopamine-dependent pathways.
When dopamine drops and iron support is insufficient, the nervous system fails to suppress background sensory noise. This breakdown is what drives nighttime restlessness, tingling, and the strong urge to move.
Root Causes Most Articles Do Not Explain Well
Central Nervous System Dysregulation
At its core, RLS is a problem of nervous system regulation. The sensory and motor areas of the brain become locked in a hyperexcitable loop. Normal sensations that would typically be ignored are perceived as urgent signals requiring movement.
This explains why walking, stretching, or shifting positions provides temporary relief. Movement activates motor pathways that override abnormal sensory input. Once movement stops, the faulty signaling returns.
Iron Deficiency Without Anemia
One of the most overlooked contributors to RLS is iron deficiency at the brain level without full-body anemia. Standard blood tests often focus on hemoglobin, which can remain normal even when iron stores are insufficient for neurological function.
Ferritin is a better marker for RLS. Research consistently shows that ferritin levels below approximately 75 ng/mL are associated with increased RLS severity. Iron is needed to support dopamine synthesis and transport in the brain, and low brain iron disrupts this process long before anemia develops.
Mineral and Vitamin Imbalances
Several nutrients influence nerve signaling and muscle relaxation:
- Magnesium helps regulate nerve excitability and muscle tone. Low magnesium increases sensory sensitivity and restlessness.
- Vitamin B12 supports nerve insulation and signal clarity. Deficiency can worsen tingling and abnormal sensations.
- Vitamin D plays a role in dopamine regulation and sleep quality. Low levels are common in people with chronic RLS symptoms.
Secondary RLS
RLS can also develop as a secondary condition. Common triggers include pregnancy, particularly in the third trimester, chronic kidney disease, and medications such as certain antidepressants, antipsychotics, and sedating antihistamines. In these cases, addressing the underlying cause is essential for lasting relief.
Research and Clinical Evidence Supporting RLS Treatment Approaches
Large, evidence-based reviews published in Movement Disorders have consistently established Restless Leg Syndrome as a neurological condition driven by dopaminergic dysfunction and altered iron handling in the brain.
A comprehensive review by Trenkwalder and colleagues (2008) demonstrated that RLS follows a clear circadian pattern, with symptoms worsening in the evening and at night due to changes in dopamine signaling and impaired sensory inhibition. The authors also emphasized that iron deficiency affecting the central nervous system can exist even when standard blood tests appear normal, highlighting the importance of evaluating ferritin rather than relying solely on hemoglobin levels.
An updated international review led by Winkelmann and colleagues (2018) reinforced these findings and refined clinical guidance for treatment. This revised analysis confirmed that non-pharmacologic strategies and correction of underlying contributors such as iron deficiency are appropriate first-line approaches for mild to moderate RLS, with medications reserved for more severe or refractory cases.
Lifestyle Adjustments That Reduce RLS Severity
Sleep Timing and Circadian Anchors
Consistent sleep timing is one of the most powerful non-medication strategies for RLS. A fixed wake-up time helps stabilize dopamine rhythms and trains the nervous system to downshift more smoothly at night.
Morning light exposure is equally important. Natural light shortly after waking strengthens circadian signaling and reduces nighttime neurological confusion. Irregular schedules, late nights, and sleeping in on weekends often worsen symptoms.
Exercise That Helps Without Triggering Symptoms
Movement is beneficial, but timing and intensity matter. Moderate exercise earlier in the day improves circulation and nervous system regulation. Walking, swimming, and gentle cycling are generally helpful.
High-intensity workouts in the evening can worsen symptoms by overstimulating the nervous system and increasing dopamine fluctuations close to bedtime. Stretching and light movement are better choices at night.
Substances That Aggravate RLS
Several common substances increase nervous system excitability:
- Caffeine stimulates dopamine release earlier in the day and worsens nighttime rebound symptoms
- Alcohol disrupts sleep architecture and increases nighttime awakenings
- Nicotine increases sensory sensitivity and delays nervous system relaxation
Certain medications, including some antidepressants and antihistamines, may also exacerbate RLS and should be reviewed with a healthcare provider.
At-Home Physical Relief Techniques
Temperature Therapy
Temperature-based strategies can provide short-term relief. Heat increases blood flow and relaxes muscles, which helps some individuals. Cold reduces nerve firing and sensory overload, which helps others. The choice depends on whether symptoms feel tight and achy or buzzy and electric.
Massage and Compression
Deep pressure activates mechanoreceptors that compete with abnormal sensory signals. Massage, compression socks, or weighted blankets can temporarily quiet the nervous system and reduce urgency.
Stretching Protocols That Work
Slow, controlled stretching is more effective than aggressive stretching. Focus areas include:
- Calves to reduce lower-leg nerve tension
- Hamstrings to decrease spinal nerve pull
- Hip flexors to improve pelvic and lumbar nerve balance
Rapid or forceful stretching often increases symptoms by overstimulating sensory pathways.
Nervous System–Focused Therapies for Restless Leg Syndrome
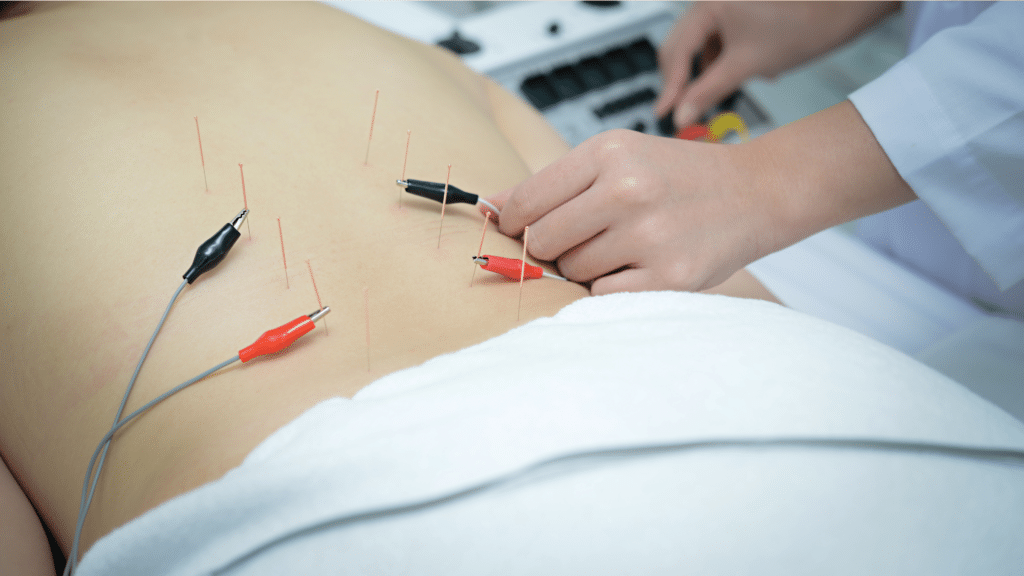
Restless Leg Syndrome improves when therapies address the nervous system rather than the legs alone. Clinical approaches that calm sensory-motor signaling, support dopamine regulation, and improve parasympathetic activity can significantly reduce nighttime urges and restlessness.
Several non-pharmaceutical therapies are commonly used to support this process, including:
- Acupuncture, which modulates dopamine pathways, reduces sensory hyperexcitability, and calms spinal reflex loops involved in involuntary movement
- Electroacupuncture or gentle neuromodulation, which provides consistent input to stabilize erratic nerve signaling in moderate to severe cases
- Manual therapy and therapeutic massage, which activate mechanoreceptors that compete with abnormal sensory signals and reduce nighttime urgency
- Targeted relaxation and breathing therapies, which shift the nervous system out of a heightened alert state and improve sleep onset
- Sleep-focused nervous system retraining, which helps restore proper downshifting at night through timing, sensory reduction, and autonomic balance
These therapies work synergistically by lowering overall nervous system noise, making it easier for the brain to suppress unnecessary movement signals during rest.
What Patients Typically Notice Over Time
Rather than immediate symptom elimination, improvement tends to follow a predictable pattern when nervous system–based therapies are applied consistently.
Early changes often include:
- Reduced intensity of leg urges in the evening
- Longer periods of stillness before symptoms appear
- Fewer nighttime awakenings related to restlessness
With continued care over several weeks, many individuals experience:
- Improved sleep continuity and duration
- Less reliance on movement to relieve symptoms
- Greater overall nervous system calm at night
The goal of these therapies is not short-term suppression, but long-term regulation. By improving how the nervous system processes sensory input and transitions into rest, nighttime symptoms become easier to manage and, in many cases, significantly less disruptive.
A Smarter, Nervous System–Focused Path to RLS Relief
Restless Leg Syndrome is best understood as a nervous system condition rather than a problem in the legs themselves. Symptoms improve when sensory signaling is calmed, neurological rhythms are stabilized, and underlying contributors such as iron or nutrient deficiencies are addressed.
When the nervous system is supported instead of suppressed, nighttime restlessness becomes easier to manage and sleep quality improves. At ACA Acupuncture and Wellness, our approach focuses on nervous system regulation and individualized care to support lasting relief and more restful nights.
Source:
Winkelmann, J., Allen, R. P., Högl, B., Inoue, Y., Oertel, W., Salminen, A. V., Winkelman, J. W., Trenkwalder, C., & Sampaio, C. (2018). Treatment of restless legs syndrome: Evidence‐based review and implications for clinical practice (Revised 2017). Movement Disorders, 33(7), 1077–1091. https://doi.org/10.1002/mds.27260
Trenkwalder, C., Hening, W. A., Montagna, P., Oertel, W. H., Allen, R. P., Walters, A. S., Costa, J., Stiasny‐Kolster, K., & Sampaio, C. (2008). Treatment of restless legs syndrome: An evidence‐based review and implications for clinical practice. Movement Disorders, 23(16), 2267–2302. https://doi.org/10.1002/mds.22254
Frequently Asked Questions
What immediately helps restless leg syndrome?
Immediate relief often comes from movement, such as walking or gentle stretching, which temporarily overrides abnormal sensory signals. Applying heat or cold, massaging the legs, or using compression can also calm symptoms short term. These methods do not fix the cause but can reduce urgency enough to fall asleep.
How to treat restless leg syndrome in kids?
Treatment in children focuses first on sleep routine consistency, adequate iron intake, and reducing overstimulation before bed. Iron deficiency is a common contributor in pediatric RLS and should be evaluated by a clinician. Medications are rarely first-line and are used only when symptoms are severe and persistent.
How to get rid of restless leg syndrome while pregnant?
Pregnancy-related RLS is often linked to increased iron demands and usually improves after delivery. Gentle movement, stretching, good sleep timing, and iron supplementation when medically indicated are the main strategies. Any supplement or treatment during pregnancy should be guided by a healthcare provider.
What is my body lacking if I have restless leg syndrome?
Many people with RLS have low iron availability in the brain, even when standard blood tests appear normal. Deficiencies in magnesium, vitamin B12, or vitamin D may also worsen symptoms by increasing nerve excitability. Identifying and correcting deficiencies is more effective than supplementing blindly.
What is the root cause of restless leg syndrome?
The root cause of RLS is dysfunction in how the nervous system regulates movement and sensory input, particularly involving dopamine signaling. Low brain iron plays a key role by disrupting dopamine production and transport. This combination leads to increased sensory noise and urges to move, especially at night.
What is the home remedy for leg pain at night?
Home strategies include light stretching, massage, heat or cold therapy, and reducing evening caffeine or alcohol. Improving sleep timing and keeping a consistent wake-up schedule also reduces nighttime symptoms. These approaches help calm the nervous system and lower symptom intensity, even if they do not eliminate RLS entirely.
Contact ACA Acupuncture & Wellness
Get in Touch
Newsletter Sign Up
LOCATIONS
MANHATTAN
QUEENS
NEW JERSEY
CALIFORNIA
ACA Franchise Opportunities
The over $4 billion US acupuncture market offers a great opportunity with over 10% annual growth rates and a continuing flow of new patients interested in the benefits of acupuncture.