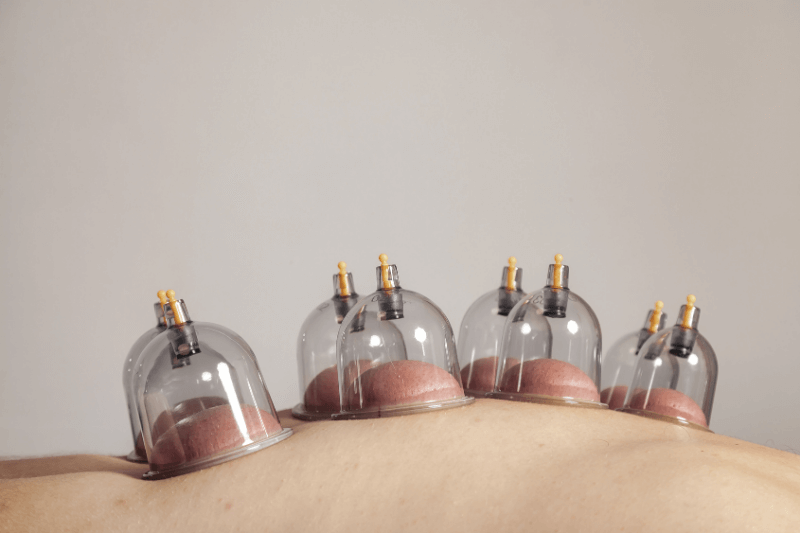
CPT Code for Cupping Therapy: Billing, Coverage, and Documentation
There is no dedicated CPT code for cupping therapy, and billing depends entirely on how the technique is performed, documented, and interpreted by the payer.
Cupping therapy is widely used in acupuncture, physical therapy, and integrative medicine settings, yet it remains one of the most misunderstood services from a billing and compliance standpoint. The coacnfusion does not come from poor clinical clarity. It comes from attempting to force a traditional therapy into a CPT system that was never designed to name or recognize “cupping” as a standalone procedure.
Understanding how cupping fits into CPT logic is essential not only for reimbursement, but for avoiding denials, audits, and post-payment recoupments.
CPT Code for Cupping Therapy: Billing, Coverage, and Documentation
There is no dedicated CPT code for cupping therapy, and billing depends entirely on how the technique is performed, documented, and interpreted by the payer.
Cupping therapy is widely used in acupuncture, physical therapy, and integrative medicine settings, yet it remains one of the most misunderstood services from a billing and compliance standpoint. The coacnfusion does not come from poor clinical clarity. It comes from attempting to force a traditional therapy into a CPT system that was never designed to name or recognize “cupping” as a standalone procedure.
Understanding how cupping fits into CPT logic is essential not only for reimbursement, but for avoiding denials, audits, and post-payment recoupments.
Key Takeaways
- There is no CPT code specifically named for cupping therapy.
- Coding depends on technique, level of provider involvement, and clinical intent.
- CPT 97016 and 97140 are most commonly used, but only in specific scenarios.
- Unlisted codes are often the most compliant option, despite lower reimbursement.
- Strong documentation is mandatory to support medical necessity and reduce risk.
Is There a Specific CPT Code for Cupping Therapy?
No CPT code explicitly names or defines cupping therapy.
CPT codes describe procedures and techniques, not traditional therapy names. Because cupping is a method rather than a defined CPT service, providers must select a code that most accurately reflects how cupping was performed and why it was clinically indicated.
This is why cupping is coded differently across clinics, disciplines, and payers. It is also why copying another provider’s billing approach without understanding the underlying logic creates compliance exposure.
Commonly Used CPT Codes for Cupping Therapy
CPT 97016 – Vasopneumatic Device
Best used for static or device-based cupping that does not require continuous provider contact.
97016 describes the application of a vasopneumatic or pressure-based modality. Many payers interpret mechanical or suction-based cupping under this code, particularly when the intent is to address edema, circulation, or post-injury swelling.
Key considerations:
- Often treated as a supervised modality, not billed in timed units
- More defensible when a mechanical suction device is used
- Coverage varies widely by payer
This code is most frequently accepted in workers’ compensation or motor vehicle accident claims when cupping is tied to injury recovery.
CPT 97140 – Manual Therapy Techniques
Appropriate only when cupping involves active, hands-on manual movement and meets time-based criteria.
97140 is a 15-minute, time-based code intended for manual techniques such as mobilization, manipulation, or soft-tissue work. Sliding or dynamic cupping, often described as myofascial decompression, may qualify only when the provider is actively engaged throughout the time billed.
Important compliance distinctions:
- Static cupping does not meet the definition of manual therapy
- Time must be clearly documented
- Must be distinct from other manual therapy billed the same day
This code is frequently audited, particularly when used for passive modalities.
CPT 97124 – Massage Therapy
Sometimes appropriate when cupping is used as a massage-style soft-tissue technique.
When cupping is performed manually for relaxation, circulation, or muscle tension relief and clearly functions as soft-tissue massage, some payers accept 97124.
This code is underutilized but can be more defensible than 97140 in certain scenarios, particularly when the therapeutic intent is not joint or motion-based.
CPT 97039 – Unlisted Modality / CPT 97139 – Unlisted Therapeutic Procedure
The most technically accurate option when cupping does not fit defined codes.
Unlisted codes exist specifically for services that lack a CPT definition. Manual cupping often falls into this category.
Reality check:
- Requires detailed documentation submitted with the claim
- Frequently denied or manually reviewed
- Often reimbursed inconsistently
Despite lower reimbursement rates, unlisted codes carry lower audit risk when used appropriately.
Choosing the Correct CPT Code Based on Technique
- Static cupping with cups left in place: 97016 or unlisted
- Sliding or moving cupping with continuous provider contact: 97140 (with strict documentation)
- Massage-style cupping for soft-tissue relaxation: 97124
- Spa or wellness cupping without diagnosis: Self-pay
The technique, not the tradition, determines the code.
Billing and Coverage Realities
Medicare and Government Payers
Medicare does not recognize cupping as a covered service. In most cases, cupping is considered non-covered or investigational. Billing Medicare for cupping creates significant compliance risk, and cash-pay is typically the safest option.
Commercial Insurance
Commercial payer policies vary. Some reimburse under 97016 or 97140 when medical necessity is well documented. Others explicitly exclude cupping regardless of code selection.
Verification is essential before billing.
Workers’ Compensation and Motor Vehicle Accident Claims
These payers are more likely to reimburse cupping when it is clearly linked to injury recovery, swelling reduction, or functional restoration and documented accordingly.
Cupping Performed With Acupuncture
Cupping is often considered bundled when performed as part of an acupuncture session. Separate billing may be defensible only when:
- The service is timed and distinct
- It targets a separate clinical goal
- Documentation clearly separates services
Modifiers may be required, but they do not override lack of medical necessity.
Documentation Requirements That Matter
Strong documentation is the difference between payment and denial.
At minimum, include:
- ICD-10 diagnosis and functional limitation
- Type of cupping and method used
- Specific body regions treated
- Time spent when using timed codes
- Patient response and plan of care integration
Example Documentation Language
97016 Example:
“Applied mechanical suction cupping to right ankle for post-sprain edema to improve circulation and reduce swelling. Duration 10 minutes. Patient tolerated well with reduced tightness noted.”
97140 Example:
“Performed dynamic sliding cupping to bilateral lumbar paraspinals for 15 minutes to address soft-tissue restriction and limited flexion. Patient reported pain reduction from 6/10 to 3/10.”
Common Billing Mistakes to Avoid
- Billing static cupping as manual therapy
- Missing time documentation
- Assuming coverage without verification
- Treating cupping as a diagnosis rather than a technique
Cash-Pay vs Insurance Billing Strategy
Many clinics choose to offer cupping as a self-pay add-on or bundle it into care packages. This approach:
- Reduces denial risk
- Simplifies compliance
- Improves patient transparency
In our acupuncture practice at ACA, we prioritize clarity, compliance, and patient trust over chasing uncertain reimbursement.
Who Defines CPT Codes and Coverage?
CPT codes are maintained and updated by the American Medical Association, which establishes standardized descriptions for medical procedures and services used in billing and reporting. These codes define how a service is categorized, but they do not determine whether the service will be paid.
Coverage and reimbursement decisions are made separately by the Centers for Medicare & Medicaid Services and by individual commercial insurance carriers. Each payer applies its own medical necessity criteria, coverage policies, and reimbursement rules, even when the same CPT code is used.
This separation means a service can be coded correctly and still be denied based on payer policy. Understanding this distinction is critical for evaluating billing risk, setting patient expectations, and deciding when a service such as cupping is better offered as a self-pay option rather than billed to insurance.
CPT Coding and Coverage Takeaways for Cupping Therapy
Cupping therapy does not face billing challenges because it lacks clinical value. Issues arise when CPT coding is misaligned with the technique performed or when payer coverage rules are misunderstood. The safest and most compliant approach is to select codes based on how cupping is delivered, document each session with clinical precision, and recognize when a cash-pay model offers greater transparency and lower risk.
When applied and documented correctly, cupping remains a valuable therapeutic tool rather than a billing liability. At ACA Acupuncture and Wellness, we offer cupping therapy as part of a broader integrative care approach alongside acupuncture, Chinese herbal medicine, TuiNa massage, physiotherapy treatment, moxibustion, reflexology, ear seeding, and access to our thermal therapy room. Our therapies may be used individually or combined within a personalized treatment plan based on each patient’s condition and goals. If you have questions about cupping therapy or whether it may be appropriate for your care, we invite you to contact us to learn more about our holistic services.
Frequently Asked Questions
Can cupping therapy ever be billed as a preventive or wellness service?
Cupping therapy is not recognized as a preventive service under CPT or insurance guidelines. Preventive benefits are typically limited to services explicitly defined by payer policy, such as screenings or vaccinations. When cupping is performed for general wellness, relaxation, or performance enhancement, it does not meet medical necessity criteria. In these cases, cupping should be clearly designated as a self-pay service.
Does the provider’s license affect which CPT code can be used for cupping?
Yes, the provider’s license significantly affects which CPT codes may be billed. Physical therapists, chiropractors, and physicians may have broader latitude to bill manual therapy or modality codes than acupuncturists, depending on payer rules. Some payers restrict codes like 97140 to specific provider types regardless of technique. Always confirm both scope of practice and payer policy before selecting a code.
Can cupping be billed if it is performed by an assistant or technician?
In most cases, cupping performed by an assistant cannot be billed under codes requiring skilled, one-on-one provider involvement. Codes such as 97140 require direct provider participation and cannot be delegated. Even supervised modality codes may have payer-specific rules regarding who may apply the treatment. Improper delegation is a common trigger for audits and recoupments.
How do insurers differentiate cupping from myofascial release during audits?
Insurers focus on provider involvement, technique description, and therapeutic intent rather than terminology. Myofascial release typically involves continuous, hands-on tissue engagement, while cupping may be passive or device-based. If documentation describes cups being placed and left unattended, it undermines manual therapy billing. Clear language describing active movement, resistance, or tissue manipulation is critical when differentiating the two.
Can cupping be billed more than once in the same treatment plan?
Cupping may be billed across multiple visits if each session is medically necessary and supports measurable progress toward functional goals. Repeated billing without documented improvement increases denial and audit risk. Insurers expect periodic reassessment and justification for continued use of the same modality. Cupping should evolve or taper as the patient’s condition changes.
What happens if a payer retroactively denies cupping claims after payment?
If a payer retroactively denies claims, they may issue a recoupment request requiring repayment of funds. Clinics are typically given a limited window to appeal with supporting documentation. Weak notes, incorrect code selection, or lack of medical necessity significantly reduce appeal success. This is why conservative coding and clear documentation are essential even when claims initially pay.
Contact ACA Acupuncture & Wellness
Get in Touch
Newsletter Sign Up
LOCATIONS
MANHATTAN
QUEENS
NEW JERSEY
CALIFORNIA
ACA Franchise Opportunities
The over $4 billion US acupuncture market offers a great opportunity with over 10% annual growth rates and a continuing flow of new patients interested in the benefits of acupuncture.